Endometrial ablation has emerged as a widely accepted and minimally invasive treatment for heavy menstrual bleeding (HMB). In fact, more than 600,000 endometrial ablations are now performed annually in the U.S. alone.1
As endometrial ablation devices have evolved, there are more options available on the market. Each device has its own risks and benefits. Here, we will compare two current and very common methods for performing endometrial ablation: heat-based thermal ablation and cryoablation.
Hyperthermic—or heat-based— thermal ablation relies on elevated temperatures to destroy the lining of the uterus. There are several types of heat-based thermal ablation treatments which were primarily used in the development of second-generation devices. These include the use of:
Broadly, all of the above can be categorized into three types of endometrial ablation treatment: gas-based thermal ablation, liquid-based thermal ablation, or wavelength/radiofrequency-based thermal ablation.
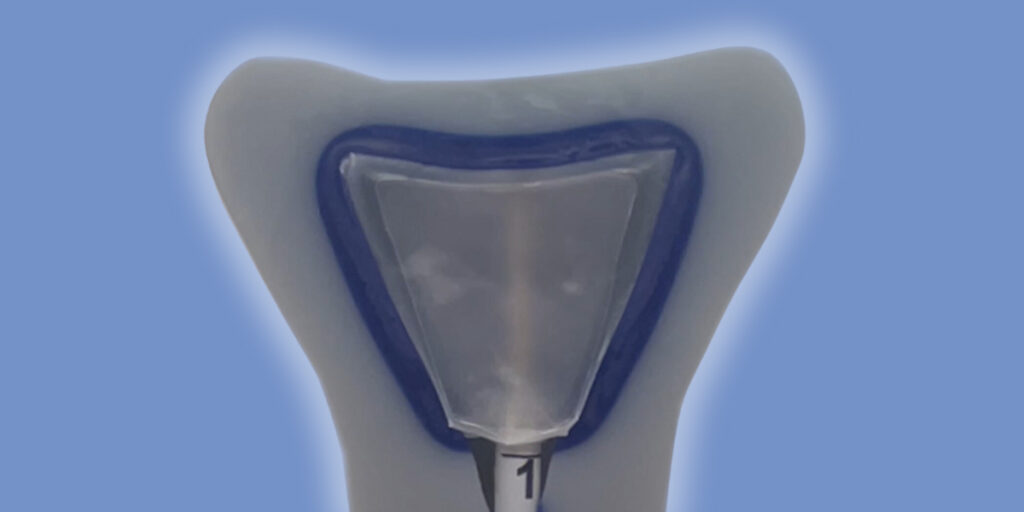
Cryoablation is a well-characterized therapy routinely used to ablate human tissues. Cryotherapy devices work by freezing the lining of the uterus in order to significantly reduce future menstrual bleeding. During this procedure, a small probe is inserted into the uterus to deliver a freezing agent that destroys the endometrium.
Cryotherapy enables:
Now let’s look at how both heat-based thermal ablation and cryoablation are used for endometrial ablation as well as the benefits and drawbacks of each.
How They WorkThe biggest difference between thermal ablation and cryoablation is the method utilized to destroy the cells of the endometrium. Heat-based thermal ablation uses extreme heat to induce cell damage and death. These therapies use elevated tissue temperatures induced by focused, high-intensity ultrasound, radiofrequency, laser, or even circulating hot water.
In contrast, cryoablation uses extreme cold to destroy the endometrium. Freezing is an energy-deprivation strategy that causes intracellular and extracellular ice formation which ultimately leads to cell dehydration and death. Fibroblasts and collagen fiber typically survive during cryotherapy, which is important for preservation of normal tissue architecture and tissue repair. Studies have shown that the tissue healing response after cryoablation can result in minimal intrauterine adhesions and preserved endometrial cavity access.2,3
Ability to Preserve Cavity AccessDue to the way heat-based thermal ablation destroys the endometrium, intracavitary scarring, adhesions and contracture inside the uterus are an expected part of the healing process post-procedure. Intracavitary scarring can lead to long term complications, such as: central or cornual hematometra, post-ablation tubal sterilization syndrome (PATSS), retrograde uterine bleeding potentially leading to the development of endometriosis, and the possible delay in diagnosis of an endometrial cancer.4 In particular, radiofrequency ablation (RFA), which makes up the majority of GEA (73%) performed annually in the US, has been associated with a high rate of post-ablation intrauterine synechiae, which may limit the ability to adequately evaluate the endometrium by biopsy or hysteroscopy to address subsequent abnormal uterine bleeding (AUB).4 In fact, a 2009 study found that endometrial biopsy failed in 23% of women with a history of thermal endometrial ablation due to endometrial assessment being compromised.5
Cryothermal energy ablates the tissue without desiccation and collagen denaturation. Post-cryoablation healing has demonstrated minimized intra-cavitary scarring, adhesions and contracture.4 Investigators in the CLARITY Study were able evaluate the uterine cavity for pathologic changes in 96% of subjects with accessible uterine cavities at 12 months.4 This is important because it allows physicians to evaluate for any new gynecologic issues in the future, such as spotting/bleeding, cyclic pelvic pain or endometrial cancer.
Analgesic EffectsFor most heat-based ablation technologies, common anesthetic and analgesic protocols in the office fail to provide enough pain relief.6
Along with a variety of physical and mental strategies used to relieve pain and anxiety both before and after ablation, cryoablation delivers additional pain management during the procedure itself. Endometrial cryoablation leverages cooling technology to ablate the endometrium while simultaneously freezing the sensory nerves supplying the uterus for an enhanced analgesic effect.7
Of course, choosing between cryoablation and thermal ablation will depend on your patient’s unique medical needs and their comfort level with the various devices and types of treatment. However, cryoablation does provide some clear advantages over thermal ablation when it comes to treating heavy menstrual bleeding:
To learn more about the Cerene Cryotherapy Device, please visit our website here.
References:
Important Safety Information
Cerene® Cryotherapy Device is indicated to ablate the endometrial lining of the uterus in premenopausal women with heavy menstrual bleeding due to benign causes for whom childbearing is complete. Pregnancy following the Cerene procedure can be dangerous; therefore, contraception must be used until menopause. The Cerene procedure is not for those who have or suspect uterine cancer; have an active genital, urinary or pelvic infection; or an IUD. There are risks and considerations associated with the use of the Cerene Cryotherapy Device. Temporary side effects may include uterine cramping, vaginal infection, and lightheadedness. For detailed benefit and risk information, consult the Cerene Instructions for Use (IFU) or your healthcare professional. CAUTION: Federal (USA) law restricts this device to sale by or on the order of a physician trained in the use of the Cerene Cryotherapy Device.
@2023 Channel Medsystems, Inc. All rights reserved. Cerene and the Channel Medsystems logo are registered trademarks of Channel Medsystems, Inc. CC-23-0111 Rev. A
Important Safety Information
Cerene® Cryotherapy Device is indicated to ablate the endometrial lining of the uterus in premenopausal women with heavy menstrual bleeding due to benign causes for whom childbearing is complete. Pregnancy following the Cerene procedure can be dangerous; therefore, contraception must be used until menopause. The Cerene procedure is not for those who have or suspect uterine cancer; have an active genital, urinary or pelvic infection; or an IUD. As with all surgical procedures, there are risks and considerations associated with the use of the Cerene Cryotherapy Device. Temporary side effects may include cramping, nausea, vomiting, vaginal discharge and spotting. For detailed benefit and risk information, consult the Cerene Instructions for use (IFU) or your healthcare professional. Learn More
